While it sounds like a profound contradiction, a catastrophic cyber-attack can serve as a powerful and unwelcome catalyst, forcing a healthcare institution to confront its deepest vulnerabilities and emerge stronger, more efficient, and fundamentally more secure. The 2022 ransomware attack on Japan’s Osaka General Medical Center provides a compelling real-world case study of this brutal but effective transformation. It turned a moment of absolute crisis, where patient care was thrown back into a pre-digital era, into a crucible for forging a comprehensive technological and cultural overhaul. The event demonstrated that the path to a more resilient future is sometimes paved with the ruins of the past, forcing an organization to not just rebuild what was lost, but to build something far better in its place. This journey from digital paralysis to a state of advanced operational security offers critical lessons for the entire healthcare industry, highlighting how the response to a disaster can ultimately redefine an institution’s capacity for excellence and innovation in patient care.
The Anatomy of a Crisis
A Digital Collapse
The ordeal at Osaka General Medical Center began with a deceptively simple sign: a slow computer on an otherwise normal October morning. This minor annoyance was the first tremor of a seismic shock that would, within two hours, bring the sprawling medical facility to its knees. A sophisticated ransomware attack had successfully breached the hospital’s defenses, severing access to its entire digital nervous system. The systems for electronic medical records, patient management, and internal communications were encrypted and rendered inaccessible, plunging the modern hospital into an abrupt and chaotic digital blackout. This sudden technological collapse forced clinicians and administrative staff into a disorienting reversion to an archaic system of handwritten paper records. The transition was jarring and fraught with risk, as the precision, speed, and collaborative potential of digital workflows vanished overnight, replaced by the slow, error-prone, and siloed nature of manual documentation. The immediate operational fallout was severe, creating a bottleneck that rippled through every department and function of the institution, threatening the continuity and quality of patient care.
The impact of the digital shutdown was felt most acutely in the hospital’s public-facing services. Serving an average of 1,300 outpatients daily, the medical center had no choice but to halt all non-essential treatments, cancel scheduled operations, and suspend new emergency admissions to prevent the chaotic internal situation from spiraling into a larger public health crisis. While the 865-bed inpatient care and the most critical emergency surgeries continued, the teams responsible for this care were operating under immense strain. The reliance on paper-based processes during the first week created a fog of confusion and anxiety, as doctors and nurses struggled to track patient histories, medication schedules, and treatment plans without the aid of centralized digital records. The hospital lobby became crowded and tense as staff struggled to manage the disruption. It was a grueling battle against time and inefficiency, and it took over two months of relentless effort for the medical center to fight its way back to a state of fully restored, normal operations. This extended period of disruption served as a stark and painful reminder of the profound dependency modern healthcare has on its digital infrastructure and the devastating consequences of its failure.
Uncovering the Cracks in the Foundation
A thorough post-mortem investigation into the attack began by tracing the digital breadcrumbs back to their source, revealing an initial point of entry that was both surprising and distressingly common in complex organizational ecosystems. The breach did not originate from a direct assault on the hospital’s primary defenses but from a seemingly peripheral and trusted partner: a third-party vendor responsible for supplying patient meals. The attackers first compromised the vendor’s server and then exploited a pre-existing external network link to pivot into the hospital’s own network. This infiltration method demonstrated that the hospital’s digital perimeter was far more porous than its security posture assumed, highlighting a critical oversight in managing supply chain vulnerabilities. The incident proved that in an interconnected world, an organization’s security is only as strong as that of its weakest partner, and the failure to secure these external connections provided the attackers with the foothold they needed to launch their devastating internal assault.
Once inside the network, the ransomware was able to propagate with astonishing speed and efficacy, a spread that was enabled not by sophisticated hacking techniques but by a series of fundamental internal failures in cybersecurity hygiene. According to the hospital’s chief information officer, the “biggest problem” was the pervasive and deeply ingrained practice of using common, shared passwords across multiple servers. This single point of failure acted as a master key for the attackers, allowing the ransomware to move laterally beyond the initially compromised server and encrypt a vast array of vital systems, including the servers housing the invaluable electronic medical records. This catastrophic spread was a direct result of a flawed security philosophy, one that was common among many Japanese hospitals at the time. This philosophy was built on the dangerously false assumption that sensitive data like medical records were inherently safe by virtue of being in a “closed environment,” supposedly isolated from the public internet. The attack shattered this myth, proving that no network is truly closed. This cultural complacency was further compounded by a general lack of understanding among staff about critical network components like VPNs and firewalls, which led to a failure to implement or appreciate the importance of robust, continuous monitoring systems.
Forging Resilience From the Ashes
A Zero-Trust Revolution
In the aftermath of the attack, as the hospital’s leadership grappled with the long road to recovery, they arrived at a critical realization: simply restoring the old system with slightly stronger passwords would be an exercise in futility. The incident had exposed deep, systemic flaws that demanded a fundamental reinvention of the institution’s entire approach to digital security. They recognized that this crisis, however painful, presented a unique opportunity to leapfrog legacy systems and build a modern, secure, and resilient digital environment from the ground up. This led to a sweeping overhaul of their infrastructure, undertaken in partnership with Microsoft, to architect a new ecosystem rooted in a “zero-trust” security model. This modern paradigm operates on the simple but powerful principle of “never trust, always verify.” It dismantles the outdated idea of a secure internal network and a dangerous external one, instead assuming that no user or device is inherently trustworthy, regardless of its location. Under this model, every single access request is rigorously authenticated and authorized before being granted, creating a far more granular and robust defense against intrusion.
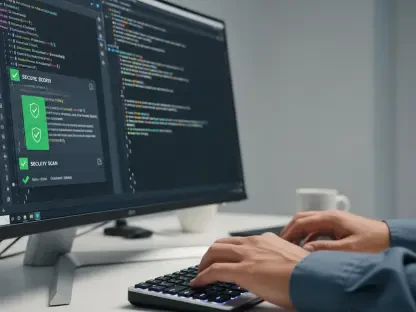
This new security-first mindset was operationalized through the implementation of a sophisticated, multi-layered defense system that permeated every aspect of the hospital’s IT. Beginning in October 2024, the hospital deployed Microsoft Defender, including its advanced Endpoint Detect and Response capabilities, to proactively identify and neutralize threats before they can cause harm. Access to the network, both for on-premises and cloud-based resources, is now managed by Microsoft Entra ID, ensuring that user identities are secure and permissions are strictly controlled. A cornerstone of this new framework is the mandatory use of multi-factor authentication for all 2,000 staff members. Employees now use a combination of security badges, chip readers, facial recognition software, and passkeys to log into the system, making it exponentially more difficult for an unauthorized user to gain access. This disciplined approach extends to daily IT operations, with the technology team now meticulously monitoring operating system updates and deploying security patches across the hospital’s vast network of 200 servers and 2,300 computers. Further strengthening this foundation, the hospital migrated a portion of its core systems—containing highly sensitive data like consultation records and prescription orders—to the Microsoft Azure cloud, leveraging the platform’s built-in security and compliance features like advanced encryption and access controls to better protect patient data.
Transforming Daily Work and Patient Care
Beyond the critical task of bolstering its defenses against future attacks, the comprehensive technological transformation has fundamentally improved the daily work and collaboration of the hospital’s staff. The enterprise-wide adoption of Microsoft 365, particularly tools like Microsoft Teams and SharePoint, has served as a powerful engine for streamlining communication, breaking down long-standing departmental silos, and fostering a new era of collaborative efficiency and innovation. For the hospital’s clinicians, the benefits of this new digital toolkit were immediate and tangible, directly impacting their ability to deliver timely and effective patient care. Dr. Haku Tanaka, a neurosurgeon, highlighted how the secure, integrated environment of Teams and SharePoint has revolutionized case consultations. He described the ability to securely share high-resolution, sensitive patient information, such as brain scan images, as invaluable for discussing complex cases like a stroke patient’s cerebral bleeding with colleagues across different departments. This represents a significant improvement over the previous reliance on phone calls, especially for a lone doctor on a night shift who needs to make critical, time-sensitive treatment decisions with the benefit of collaborative input.
This enhancement in personal and team effectiveness was echoed by other clinical leaders. Dr. Tetsuya Takao, the Head of Urology, noted a marked increase in his own efficiency and responsiveness. He can now securely access patient files and essential documents from home via Teams, enabling him to check on a patient’s condition remotely and disseminate crucial information to his entire team simultaneously with a single message. This enhanced flexibility and connectivity not only supports better, more continuous patient care but also directly addresses the pervasive issue of work-life balance, a major challenge for overworked healthcare professionals in Japan. This cultural and operational shift was also profoundly felt among the hospital’s 1,000-member nursing staff. Head Nurse Masami Murai explained how her team now uses dedicated chat groups in Teams for a wide variety of purposes, from coordinating tasks among head nurses to managing large-scale disaster response protocols. This has replaced the cumbersome and inefficient process of tracking down individual email addresses, fostering a more agile and collaborative environment that enables “bottom-up communication” and sparks ingenuity among the nurses, who now use SharePoint to create and share a repository of peer-developed training videos.
A Blueprint For the Future
Cultivating a Culture of Innovation
The newly established secure and collaborative digital environment has become a fertile ground for innovation, with the hospital actively encouraging a culture where employees are empowered to identify problems and build their own solutions. Younger staff members have been at the forefront of this movement, leading a “Young Members Teams Utilisation Project” to tackle everyday administrative inefficiencies. One of the project’s flagship achievements was the development of a digital patient feedback form using Microsoft Forms. Launched in April 2025, the system allows patients to easily submit their feedback by scanning a QR code with their smartphones. This simple yet elegant solution has significantly reduced the administrative time required to manually collect, transcribe, and process paper-based responses, freeing up staff to focus on more value-added activities. This initiative serves as a powerful example of how providing employees with the right set of modern, accessible tools can unlock their latent creativity and drive meaningful, bottom-up improvements in hospital operations.
This proactive spirit of technological adoption extends to the exploration of emerging AI tools. These same younger staff members are becoming early adopters of AI assistants like Copilot Chat, integrating them into their daily workflows to enhance productivity and decision-making. They use these tools to efficiently organize meeting notes, generate concise summaries of complex issues, and brainstorm next steps for various projects. The nursing staff has also found practical applications for AI, using it to transcribe important conversations and to double-check their work for potential omissions, such as reviewing an evaluation sheet for new hires to ensure all criteria have been addressed. This grassroots adoption is building a foundation of familiarity and trust in AI, with staff already seeing its immense potential to alleviate some of their most significant administrative burdens. Assistant Head Nurse Toshie Konaka pointed to the time-consuming and cumbersome task of manually creating nurses’ duty rosters—a complex logistical puzzle—as a prime candidate for future AI-powered automation, envisioning a future where technology handles the tedious work, allowing them to dedicate more time to direct patient interaction and care.
Navigating an Evolving Landscape
The remarkable transformation at Osaka General Medical Center occurred against the backdrop of significant structural challenges facing Japan’s entire healthcare sector. As noted by industry analysts, the nation’s aging population and low birthrate have created an ever-widening gap between the escalating demand for medical care and the shrinking supply of healthcare workers, with a projected shortfall of 250,000 professionals this year alone. This demographic pressure has been compounded by severe financial strain on public hospitals, with President Shimazu stating that approximately 80% have been operating “in the red,” making large-scale investments in new technology a difficult and often deferred decision for many institutions. In this context, the 2022 ransomware attack, while initially devastating, served as the ultimate non-negotiable catalyst for modernization. It forced an investment that, under normal circumstances, might have been delayed for years.
Ultimately, the hospital emerged from the crisis not only with a strengthened, multi-layered security framework and vastly improved work processes but also with a more collaborative and innovative culture. The institution’s journey from digital collapse to a state of advanced resilience provided it with the modern tools and efficient workflows needed to better navigate the demanding healthcare landscape. Most importantly, it cultivated a team of seasoned professionals who had been tested by a real-world disaster and had come out the other side more prepared and capable. As disaster response head Dr. Fujimi concluded, the key to navigating any crisis was preparation. The experience had forged a clear organizational structure and ensured every individual understood their role, allowing them to remain calm and execute their duties effectively under pressure. The technology was the enabler, but the true asset was the crisis-hardened team it helped create.